If persistent shoulder stiffness and pain are limiting daily life, arthroscopic capsular release for frozen shoulder in Bangalore can be a highly effective, minimally invasive solution to restore motion and relieve pain, especially when physiotherapy and medications haven’t worked. Frozen shoulder (adhesive capsulitis) involves a thickened and contracted joint capsule that restricts movement; arthroscopic release targets and frees these tight tissues through keyhole incisions to improve range of motion and function.
At Opera Bone and Joint Clinic, Malleswaram, Dr. Ponnanna K.M—Consultant Orthopaedic and Joint Replacement Surgeon—offers advanced arthroscopic shoulder care, including capsular release for frozen shoulder, with a focus on precise technique, faster recovery, and personalized rehabilitation. His practice emphasizes minimally invasive arthroscopy, patient-centered protocols, and evidence-based pathways to help patients resume daily activities with less pain and better mobility.
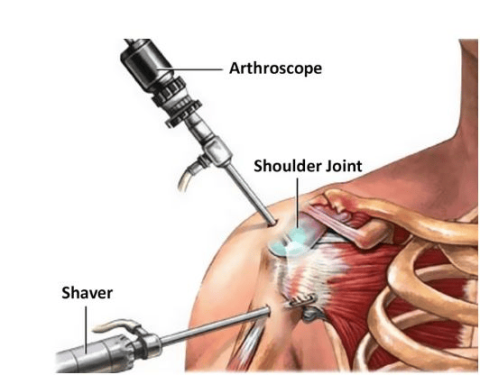
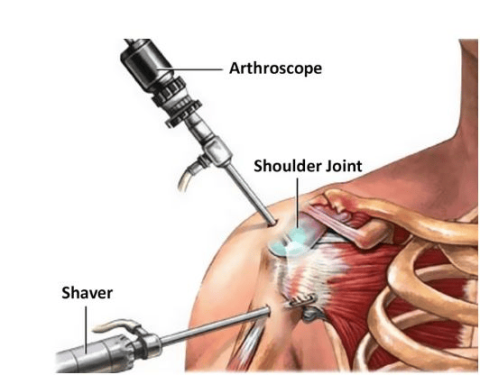
Arthroscopic capsular release is a keyhole procedure using an arthroscope (camera) and specialized instruments to visualize the shoulder and carefully incise the thickened, contracted capsule, thereby restoring space and movement inside the joint. This targeted release improves elevation and rotation, helping patients regain functional range after conservative care has plateaued.
Common contributors include prior injury or surgery with prolonged immobilization, systemic conditions like diabetes or thyroid disorders, and inflammatory diseases such as rheumatoid arthritis. Symptoms typically evolve gradually: progressive shoulder pain (often worse at night), stiffness, restricted overhead reach and external rotation, and difficulty with routine activities.
Under anesthesia, the surgeon makes small incisions, inserts the arthroscope, and releases tight capsular bands and adhesions to free the joint and restore motion, usually within 1–2 hours depending on severity. Because it’s minimally invasive, patients benefit from smaller incisions, reduced scarring, and a structured pathway to early rehab.
After surgery, pain control, sling use for comfort, wound care, and rapid initiation of guided physiotherapy are standard. Rehabilitation begins early with gentle range-of-motion work, then progresses to strengthening and flexibility as healing advances. Many patients see significant improvements within 3–6 months, with full recovery potentially taking up to a year depending on individual factors and adherence to therapy.
Benefits include improved range of motion, reduced pain, better function, smaller scars, and typically a shorter recovery than open surgery. Risks—though uncommon with expert technique—can include infection, bleeding, nerve or vessel injury, residual stiffness, anesthesia-related effects, and incomplete symptom resolution requiring further care. A specialist-led plan and diligent physiotherapy minimize complications and optimize outcomes.